ICD implantation, monitoring and battery life

How are ICDs implanted?
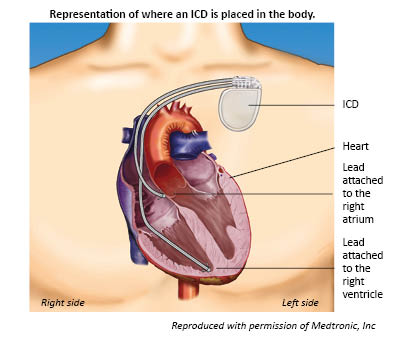
ICDs are usually implanted by an electrophysiologist (cardiologist specialising in heart rhythm disorders). They are usually implanted on the left side as this is closer to the heart for the leads to be placed.
You can ask your hospital for further information about the procedure for this, as it may vary from one hospital to another.
You would usually have the device implanted either under a general anaesthetic, or while you are sedated and under a local anaesthetic. You will usually be in hospital overnight following the implant (to check on your recovery) and given an x-ray to ensure that the ICD is correctly in place and you have no complications from the surgery.
With regular ICDs, the leads are inserted first, through a small (5-10cm long) incision under the collarbone. They are fed through a vein in the neck down into the right side of the heart. An x-ray is used to guide the leads into place. If the device has a single lead, it will be placed in the ventricle. If it has two, one sits in the ventricle and one in the atria. The leads are attached to the heart muscle to keep them in place.
The generator is then implanted. This is usually located in the left side of the upper chest, and sits in a small space under the skin or muscle (sometimes referred to as a ‘pocket’). The generator is then connected to the lead (or leads).
Once the generator and leads are in place and connected, the device will be ‘programmed’. This involves testing that the device works by bringing on an arrhythmia using electrical impulses, and checking that the device responds to treat these arrhythmias. It will also be programmed to recognise natural increases in your heart rate, such as when you are active or exercising. This is important as it means that the device can be adjusted and programmed to meet your needs.
The wound is closed with stitches and covered with a dressing.
The hospital will provide information about recovery, care of your wound and removal of stitches (which may dissolve or need to be removed - which can usually be done by your GP surgery).
If there is a reason why implanting the battery on the left side would be difficult (for example, if you are left handed) you might want to talk to your doctors about whether you could have the implant on the right side (although the wires would still go into the right side of the heart).
How are S-ICD implanted?
The process for implanting an S-ICD is similar to having an ICD, with the leads being implanted, followed by the generator. However, the generator is located lower down on the body, and the leads go under the skin (rather than along a blood vessel).
What are the risks of implantation?
As with any surgical procedure, there are some risks to having an ICD implanted. These can include the following.
- Soreness and bruising around the implant site (this can be due to the procedure which includes implanting the device under the skin). Any bruising will usually disappear in a couple of weeks.
- Risk of infection from the wound site (your doctors will explain how to clean and care for your wound to minimise this risk).
- Damage to the blood vessels as the leads are put in place.
- Damage to the lungs, where either air or blood leaks out of the lungs and into the chest cavity (which can happen as the leads are put into place). This is called a pneumothorax and may get better on its own or the air may need to be drained out.
- Blood clots due to the operation. You may be given anticoagulant medication to reduce any blood clot should this happen.
Following the procedure, complications may include the following.
- Risk of infection from the device, which can cause pain, swelling and a fever. This can happen during the first year of having the device implanted. This will usually be treated with antibiotics, and it may mean that the ICD needs to be replaced.
- Problems with the device, where it doesn’t work properly. This could be due to a fault with the leads, or the generator or battery. This might mean that the ICD needs to be re-programmed or replaced.
Although these risks may sound worrying, the likelihood of them happening is small. It is also worth considering the risks of implantation against the benefit of the ICD which can monitor and treat dangerous arrhythmias.
Your doctors will discuss these risks with you before any procedure, so you can talk through any concerns you have.
Moving around after an implant operation
You will be advised to limit the movement of your left arm for a few weeks following surgery. This means avoiding lifting your arm higher than shoulder height and avoiding strenuous activity or exercise, stretching or lifting heavy objects. Also, avoid any pressure directly on the wound or device. This is to give the leads time to become firmly attached to the heart muscle and lessens that chance that the leads will move. It also gives time for your wounds to heal.
After a couple of weeks, you can usually return to normal activities, including work, and most exercise and leisure activities. However, you may be advised to continue to avoid activities that could potentially damage the ICD (such as contact sports).
Can you see the device once it is implanted?
When you have an ICD you will have a small scar where it was implanted. This might be visible, depending on what you are wearing. Generally, devices are relatively small so, depending on your build, they may not be obvious. You may be able to feel where the device is, but again this will depend on your build. However, you may be aware of the device if you touch the area or lie in certain positions.
Some people may be aware of the device and keep touching it, even subconsciously. This is sometimes called ‘Twiddler’s syndrome’ and may cause problems if the pacemaker moves position. Although this
is very rare, in this case the device may need to be repositioned.
How is my device monitored?
If you have an ICD implanted, you will be given an appointment at an ICD clinic (often called a ‘pacing clinic’) a few weeks after the implant, to check your ICD and see how you are getting on. After this, you will need to have your device routinely monitored for as long as you have it. This is to check your ICD and whether it has treated any arrhythmias, and is a way of monitoring your condition. Your ICD contains software so that it can store information about your heart, and whether the ICD has been activated. This information can be downloaded and reviewed by the clinic. It is also when the battery of your device will be checked, so that you have plenty of warning for when it will need to be replaced.
Monitoring might be done at a clinic every six months or so (depending on how you are getting on). However, most ICD’s can now be monitored with a remote device at home, which usually sits by your bedside. This remote device uses a wireless connection to download information from your ICD, which it sends via a mobile phone network to your ICD clinic. This may mean you don’t have to attend a clinic as often as you would without remote monitoring. It can also be reassuring if you have any symptoms that you are worried about.
You can ask your doctors whether this is possible for you.
How long does an ICD last?
The battery on an ICD usually last around 5 – 10 years (depending on the individual device and how much it is used). The battery life will be monitored during your routine clinic appointments. When the battery is low the ICD will need to be replaced. The surgery for this is similar to when you had the ICD implanted, but usually only the generator needs to be changed (the leads are kept in place and attached to the new battery). The surgeons may make the incision over the top of the last one to reduce any new scarring.
©Cardiomyopathy UK. April 2018