Types of ICD

There are two types of ICD.
Regular ICDs – these are implanted under the skin on the upper chest wall, usually on the left side, and are connected via wires that pass through a blood vessel leading into the heart. These have a pacing function (for too-fast and too-slow heart rhythms) as well as being able to defibrillate (to ‘fire’ or ‘shock’ the heart).
Subcutaneous ICDs (or S-ICDs) – these are implanted on the lower left side of the chest towards the bottom of the ribs. The leads are fed under the skin (subcutaneously), across the ribs and along the breast bone to the heart. The leads do not sit within the heart (unlike a regular ICD) and so the deliver a shock to the outside of the heart (rather than within the heart). As S-ICDs do not sit within the heart
they are not currently able to offer the same pacing function as a regular ICD.
Both ICDs record details of your heart rhythm, and any activation of the device, which can be useful for monitoring your condition.
If you are considering having an ICD you can ask your doctors whether they have any patient information (such as a booklet) from the device company that they can give you to read.
There is a third device – called a CRT-D – which includes an ICD function. This is a type of pacemaker called ‘cardiac resynchronisation therapy’ device or biventricular pacemaker).
Which device would I need?
Which device you would need depends on your medical needs.
A regular ICD is smaller than an S-ICD, but it is more invasive as the leads feed through a vein and sit within the heart’s muscle walls. If the leads need replacing this is a more complicated procedure than
with an S-ICD as they can become securely embedded in the heart muscle and difficult to extract. However, this device is suitable for anyone who may need a pacing function.
An S-ICD battery is larger than a regular ICD, but the device is less invasive as the leads sit outside the heart rather than within the heart. If the leads need to be changed this is a more straightforward
operation than for a regular ICD and so it may be considered an option for people who are likely to need more lead replacements during their lifetime (for example, younger people compared to
older people). It may also be recommended for someone for whom a regular ICD is not suitable, for example if they have a condition that makes it difficult for the wires to be placed through a blood vessel into the heart. As S-ICDs do not have a pacing function they are suitable for people who do not need the additional pacing but are not suitable for someone who needs a pacing function.
Do I still need to take medication if I have an ICD?
ICDs are used to treat dangerous arrhythmias when they happen. They do not prevent arrhythmias, and they do not treat other symptoms of cardiomyopathy. If you take medication for symptoms
from your cardiomyopathy you will most likely need to continue to take these medications. The ICD is an additional form of treatment, rather than an alternative.
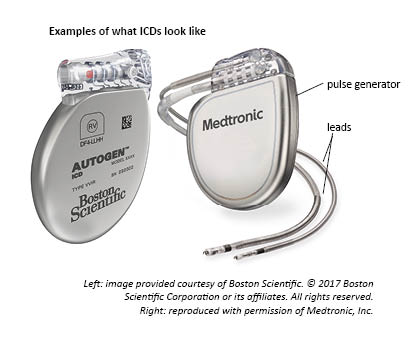
What do ICDs look like?
ICDs consist of a pulse generator (which includes a battery), which looks like a small box, and a number of leads. These leads are like fine coated wires, with special electrodes on the end, which are connected to the generator. These leads are either fed into the heart through a vein, or sit outside the heart, (depending on the type of ICD) where they monitor the heart’s rhythm. If needed, the leads deliver a shock from the generator to the heart to restore the heart’s normal rhythm.
There are several companies that make ICDs so your ICD may look slightly different to the examples below.
Deciding whether to have an ICD or not
An ICD is only recommended when it is considered necessary for you, either because you have had, or are at risk of having, potentially life-threatening arrhythmias. However, the decision whether to have
an ICD is yours, and it is important that you feel you have enough information and support to make this decision.
The decision can be difficult, and it can feel over-whelming. It may help to think about the risks and benefits of having, and of not having, the ICD. And it can help to talk through any questions or concerns you have, both with your doctors and the ICD clinic, and with those close to you.
If you would like to talk to someone with experience of having an ICD, call our helpline and ask to be put in contact with a peer support volunteer.
©Cardiomyopathy UK. April 2018